surgeries
Ureteric Stones
Procedure– A small 2 to 3 mm diameter long slender endoscope is introduced through the urethra into the ureter and the stone is fragmented or removed.
80% stones can be cleared with good success rate.
1.Limitation due to Anotomical constraints, stones migrating up.
2. Miniature or flexible URS may be required
3. C-Arm guidance.
Blader stones
1. Almost any stone can be done Endoscopically.
2. Hospital stay less than a day.
3.No pain.
4.Small stones done on OPD basis under LOCAL NAESTHESIA A.Mauer Mayer stone punch.
5.Blader stone sheath / Nephroscope.
6.Success rate almost 100%
7.Complication rate almost 0%
2. Hospital stay less than a day.
3.No pain.
4.Small stones done on OPD basis under LOCAL NAESTHESIA A.Mauer Mayer stone punch.
5.Blader stone sheath / Nephroscope.
6.Success rate almost 100%
7.Complication rate almost 0%
Antegrade PCNL
1. Large / Hard stones
2. Stones not accessible to URS.
3. Stone migration during URS.
4. Success rate very high
5. Push Bang ESWL
6. Ureterolithotomy, Retroperitoneo scopy, Laparo scopy etc.
2. Stones not accessible to URS.
3. Stone migration during URS.
4. Success rate very high
5. Push Bang ESWL
6. Ureterolithotomy, Retroperitoneo scopy, Laparo scopy etc.
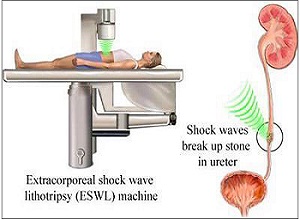
ESWL
EXTRACORPOREAL SHOCKWAVE LITHOTRIPSY Credit for the invention of LITHOTRIPSY goes to Doenier.It is a procedure wherein NO Anaesthasia is required and it is not at all an operation. The Urologist does not even touch the patient.
The patient just lies down on the Lithroscopy table, a 6 inches baloon touches the Lion and Soundwaves hit the body which feels like strong tapping on the skin. It is done on the OPD basis and the patient is called back for subsequent sittings depending upon the size and the hardness of the stone.
1. Success rate 95%
2. No admission>br> 3. Non Invasive
4. No Anaesthesia
5. Age no bar
6. Minimal side effects
1. Success rate 95%
2. No admission>br> 3. Non Invasive
4. No Anaesthesia
5. Age no bar
6. Minimal side effects
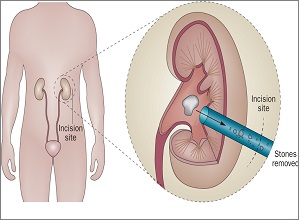
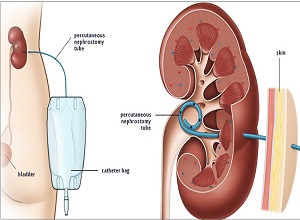
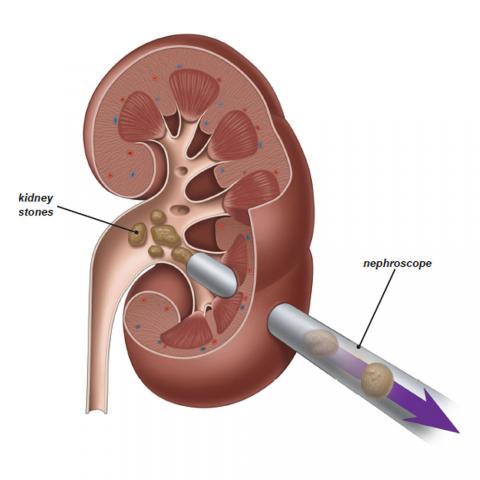
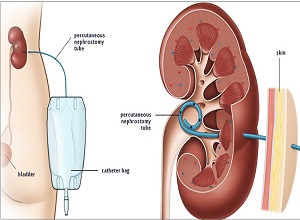
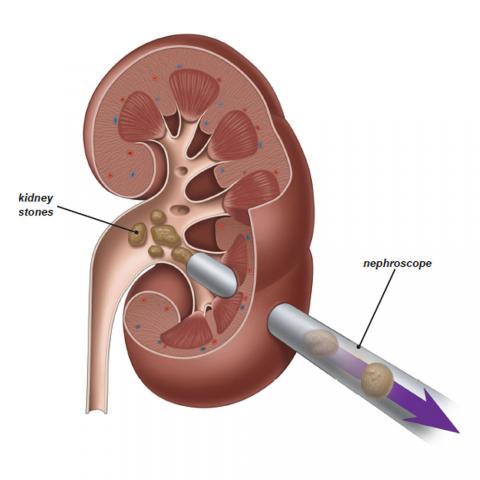
PCNL
PERCUTANEOUS NEPHROLITHOLITHOTOMY.
A small 7 to 8 mm puncture is done in the Lion under anaesthesia , endoscope is introduced through this hole into kidney, the stone is fragmented and the fragments are removed through the same hole.
1. Minimal Access Surgery
2. Stones of almost any size cleared
3. Hardness not a criteria
4. Minimal complication
5. Regional Anesthesia
6. Short hospital stay of 2 – 3 days
7. Minimal post op pain
1. Minimal Access Surgery
2. Stones of almost any size cleared
3. Hardness not a criteria
4. Minimal complication
5. Regional Anesthesia
6. Short hospital stay of 2 – 3 days
7. Minimal post op pain
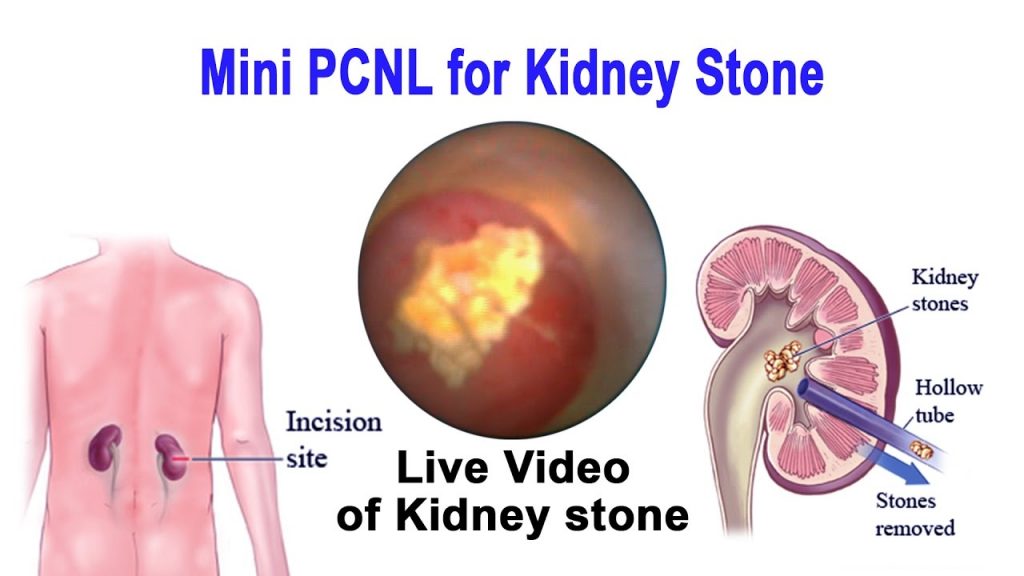
Mini percutaneous nephrolithotomy.
The minimal invasive percutaneous nephrolitholapaxy, abbreviated Mini-PCNL, is an endoscopic procedure to remove kidney stones. It is used for larger kidney stones (>1.5cm) or if other therapy methods, e.g. shock wave treatment (ESWT) or flexible ureterorenoscopy, have not been or do not seem successful due to anatomic particularities of the pelvicalyceal system.
1.Mini-PCNL constitutes an effective and very safe method to treat kidney stones. Depending on the size of the stone, repeated surgery is only very rarely required. Generally, the patient is immediately “stone-free”. The use of small instruments makes Mini-PCNL a low-risk procedure. Severe complications like heavy bleeding are extremely rare and treatable.
2. the endoscope is inserted into the kidney. Using a special laser, the kidney stones are then broken up and washed out while a direct view of the operation is provided. At the end of surgery, a catheter (hose), a so-called renal fistula, is placed in the kidney to secure the outward urine flow. This catheter can generally be removed without any pain a few days after surgery.
1.Mini-PCNL constitutes an effective and very safe method to treat kidney stones. Depending on the size of the stone, repeated surgery is only very rarely required. Generally, the patient is immediately “stone-free”. The use of small instruments makes Mini-PCNL a low-risk procedure. Severe complications like heavy bleeding are extremely rare and treatable.
2. the endoscope is inserted into the kidney. Using a special laser, the kidney stones are then broken up and washed out while a direct view of the operation is provided. At the end of surgery, a catheter (hose), a so-called renal fistula, is placed in the kidney to secure the outward urine flow. This catheter can generally be removed without any pain a few days after surgery.
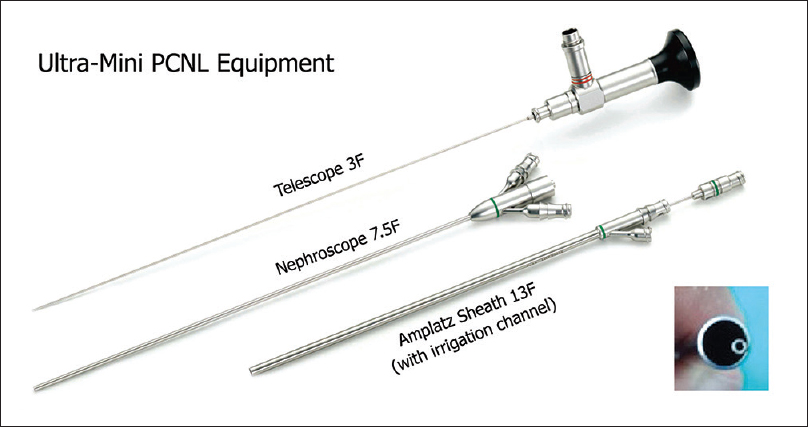
Ultra-mini-percutaneous nephrolithotomy
Since the introduction of percutaneous nephrolithotomy (PCNL) there have been various modifications to improve success rates. The overall complication rate of PCNL can be up to 83%, which can be minimised by accurate patient selection and careful postoperative follow-up. One of the most important differencesbetween the various PCNL techniques is the size of renal access (and the required specialised equipment), which contributes to the broad spectrum of complications and outcomes. Today, PCNL techniques include: standard PCNL (S-PCNL), mini-PCNL (also called mini-perc), ultra-mini-PCNL (UM-PCNL), and the recently introduced micro-PCNL. S-PCNL is the standard procedure in the treatment of renal and upper ureteric stones using a 28–30-F ureteroscope.
RIRS (retrograde intrarenal surgery)
RIRS (retrograde intrarenal surgery): Retrograde intrarenal surgery (RIRS) is a procedure for doing surgery within the kidney using a viewing tube called a fiberoptic endoscope.In RIRS the scope is placed through the urethra (the urinary opening) into the bladder and then through the ureter into the urine-collecting part of the kidney. The scope thus is moved retrograde (up the urinary tract system) to within the kidney (intrarenal).
RIRS may be done to remove a stone. The stone is seen through the scope and can then be manipulated or crushed by an ultrasound probe or evaporated by a laser probe or grabbed by small forceps, etc.
RIRS is performed by a specialist, an urologist (endourologist) with special expertise in RIRS. The procedure is usually done under general or spinal anesthesia.
The advantages of RIRS over open surgery include a quicker solution of the problem, the elimination of prolonged pain after surgery, and much faster recovery.
Ureteric Stones
Procedure– A small 2 to 3 mm diameter long slender endoscope is introduced through the urethra into the ureter and the stone is fragmented or removed.
80% stones can be cleared with good success rate.
1.Limitation due to Anotomical constraints, stones migrating up.
2. Miniature or flexible URS may be required
3. C-Arm guidance.
Blader stones
1. Almost any stone can be done Endoscopically.
2. Hospital stay less than a day.
3.No pain.
4.Small stones done on OPD basis under LOCAL NAESTHESIA A.Mauer Mayer stone punch.
5.Blader stone sheath / Nephroscope.
6.Success rate almost 100%
7.Complication rate almost 0%
2. Hospital stay less than a day.
3.No pain.
4.Small stones done on OPD basis under LOCAL NAESTHESIA A.Mauer Mayer stone punch.
5.Blader stone sheath / Nephroscope.
6.Success rate almost 100%
7.Complication rate almost 0%
Antegrade PCNL
1. Large / Hard stones
2. Stones not accessible to URS.
3. Stone migration during URS.
4. Success rate very high
5. Push Bang ESWL
6. Ureterolithotomy, Retroperitoneo scopy, Laparo scopy etc.
2. Stones not accessible to URS.
3. Stone migration during URS.
4. Success rate very high
5. Push Bang ESWL
6. Ureterolithotomy, Retroperitoneo scopy, Laparo scopy etc.
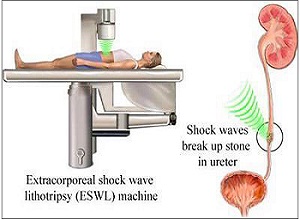
ESWL
EXTRACORPOREAL SHOCKWAVE LITHOTRIPSY Credit for the invention of LITHOTRIPSY goes to Doenier.It is a procedure wherein NO Anaesthasia is required and it is not at all an operation. The Urologist does not even touch the patient.
The patient just lies down on the Lithroscopy table, a 6 inches baloon touches the Lion and Soundwaves hit the body which feels like strong tapping on the skin. It is done on the OPD basis and the patient is called back for subsequent sittings depending upon the size and the hardness of the stone.
1. Success rate 95%
2. No admission>br> 3. Non Invasive
4. No Anaesthesia
5. Age no bar
6. Minimal side effects
1. Success rate 95%
2. No admission>br> 3. Non Invasive
4. No Anaesthesia
5. Age no bar
6. Minimal side effects
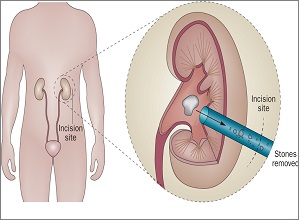
PCNL
PERCUTANEOUS NEPHROLITHOLITHOTOMY.
A small 7 to 8 mm puncture is done in the Lion under anaesthesia , endoscope is introduced through this hole into kidney, the stone is fragmented and the fragments are removed through the same hole.
1. Minimal Access Surgery
2. Stones of almost any size cleared
3. Hardness not a criteria
4. Minimal complication
5. Regional Anesthesia
6. Short hospital stay of 2 – 3 days
7. Minimal post op pain
1. Minimal Access Surgery
2. Stones of almost any size cleared
3. Hardness not a criteria
4. Minimal complication
5. Regional Anesthesia
6. Short hospital stay of 2 – 3 days
7. Minimal post op pain
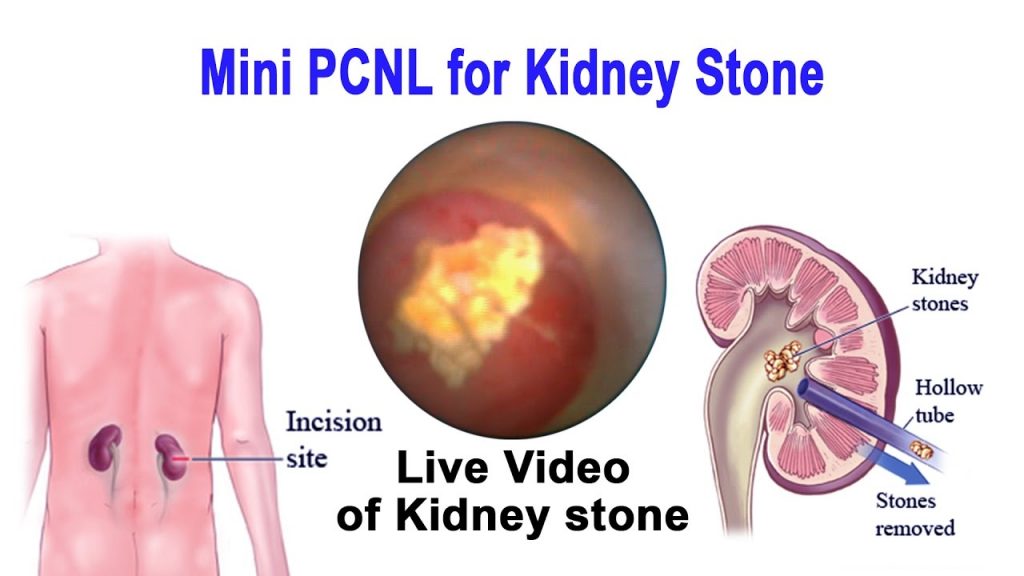
Mini percutaneous nephrolithotomy.
The minimal invasive percutaneous nephrolitholapaxy, abbreviated Mini-PCNL, is an endoscopic procedure to remove kidney stones. It is used for larger kidney stones (>1.5cm) or if other therapy methods, e.g. shock wave treatment (ESWT) or flexible ureterorenoscopy, have not been or do not seem successful due to anatomic particularities of the pelvicalyceal system.
1.Mini-PCNL constitutes an effective and very safe method to treat kidney stones. Depending on the size of the stone, repeated surgery is only very rarely required. Generally, the patient is immediately “stone-free”. The use of small instruments makes Mini-PCNL a low-risk procedure. Severe complications like heavy bleeding are extremely rare and treatable.
2. the endoscope is inserted into the kidney. Using a special laser, the kidney stones are then broken up and washed out while a direct view of the operation is provided. At the end of surgery, a catheter (hose), a so-called renal fistula, is placed in the kidney to secure the outward urine flow. This catheter can generally be removed without any pain a few days after surgery.
1.Mini-PCNL constitutes an effective and very safe method to treat kidney stones. Depending on the size of the stone, repeated surgery is only very rarely required. Generally, the patient is immediately “stone-free”. The use of small instruments makes Mini-PCNL a low-risk procedure. Severe complications like heavy bleeding are extremely rare and treatable.
2. the endoscope is inserted into the kidney. Using a special laser, the kidney stones are then broken up and washed out while a direct view of the operation is provided. At the end of surgery, a catheter (hose), a so-called renal fistula, is placed in the kidney to secure the outward urine flow. This catheter can generally be removed without any pain a few days after surgery.
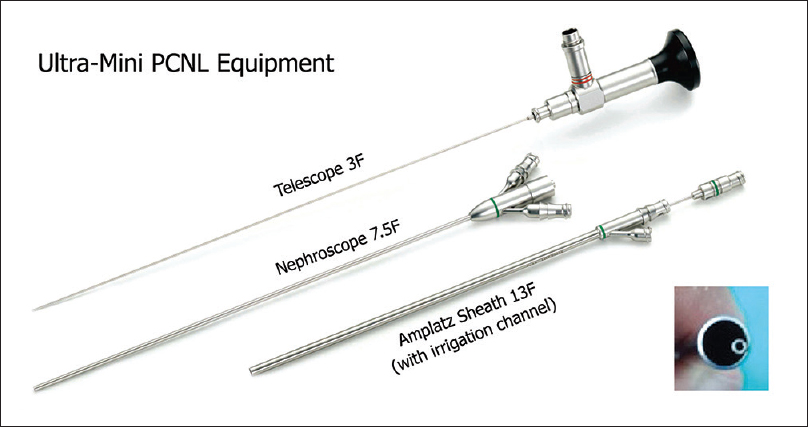
Ultra-mini-percutaneous nephrolithotomy
Since the introduction of percutaneous nephrolithotomy (PCNL) there have been various modifications to improve success rates. The overall complication rate of PCNL can be up to 83%, which can be minimised by accurate patient selection and careful postoperative follow-up. One of the most important differencesbetween the various PCNL techniques is the size of renal access (and the required specialised equipment), which contributes to the broad spectrum of complications and outcomes. Today, PCNL techniques include: standard PCNL (S-PCNL), mini-PCNL (also called mini-perc), ultra-mini-PCNL (UM-PCNL), and the recently introduced micro-PCNL. S-PCNL is the standard procedure in the treatment of renal and upper ureteric stones using a 28–30-F ureteroscope.
RIRS (retrograde intrarenal surgery)
RIRS (retrograde intrarenal surgery): Retrograde intrarenal surgery (RIRS) is a procedure for doing surgery within the kidney using a viewing tube called a fiberoptic endoscope.In RIRS the scope is placed through the urethra (the urinary opening) into the bladder and then through the ureter into the urine-collecting part of the kidney. The scope thus is moved retrograde (up the urinary tract system) to within the kidney (intrarenal).
RIRS may be done to remove a stone. The stone is seen through the scope and can then be manipulated or crushed by an ultrasound probe or evaporated by a laser probe or grabbed by small forceps, etc.
RIRS is performed by a specialist, an urologist (endourologist) with special expertise in RIRS. The procedure is usually done under general or spinal anesthesia.
The advantages of RIRS over open surgery include a quicker solution of the problem, the elimination of prolonged pain after surgery, and much faster recovery.